Health
Researcher Unveils Zika Virus Pathways to the Placenta

A groundbreaking discovery by researcher Rafael Michita at Baylor College of Medicine has illuminated the pathways through which the Zika virus infiltrates the placenta. In his postdoctoral research, which began in 2021, Michita observed thin filaments connecting infected cells to their neighbors while examining Zika viruses under a microscope. This led him to hypothesize that these intercellular connections, known as tunneling nanotubes (TNTs), might play a crucial role in the virus’s ability to breach the placental barrier, which typically protects the fetus from infections.
Determined to explore this intriguing observation further, Michita embarked on research that has positioned him as a leader in the field of maternal-fetal viral transmission. The implications of his findings extend beyond Zika, as TNTs are known to be exploited by various viruses, including HIV and SARS-CoV-2, to move between cells while evading the immune system.
Exploring Tunneling Nanotubes
The concept of tunneling nanotubes emerged in the early 2000s as a means of direct cellular communication, allowing the transfer of signaling molecules, nutrients, and organelles. However, their role in viral transmission has only recently garnered attention. Michita’s research represents one of the first attempts to link TNTs to the Zika virus, suggesting that these structures may facilitate not just cell-to-cell spread but also the transfer of mitochondria from healthy cells to infected ones, thus enhancing the virus’s replication capabilities.
According to Olena Shtanko, an assistant professor at the Texas Biomedical Research Institute, Michita’s work challenges traditional views within the scientific community. Shtanko, who previously discovered that Ebola virus utilizes TNTs, remarked, “Tunneling nanotubes are a very out-of-the-box concept that, at first, wasn’t accepted by researchers. They needed more proof.” The potential for TNTs to contribute to viral pathogenesis has opened new avenues for therapeutic strategies aimed at blocking viral transmission and protecting fetal health.
A Unique Perspective on Biology
Michita’s journey into this area of research is rooted in his diverse background. Originally from Brazil, where he specialized in genomic studies related to pregnancy disorders, Michita’s multicultural upbringing fostered a deep curiosity about biological processes from an early age. His academic path has taken him across the globe, including time spent in New Zealand and Germany, where he gained invaluable experience that enriched his understanding of immunogenetics and cell biology.
His interest in uncovering the genetic factors influencing pregnancy led him to recognize the significant gaps in knowledge regarding pregnancy-related diseases. This became especially pertinent during the Zika virus epidemic in Brazil from 2015 to 2016, which underscored the urgent need for research into how the virus impacts maternal health and fetal development. “The lack of understanding of how the virus infects the placenta, coupled with the unsettling reality that there is no cure for Zika virus, made it clear that I needed to expand my skill set,” Michita stated.
Within the laboratory led by Indira Mysorekar, Michita found an environment that encouraged innovative thinking. He was empowered to explore the intersection of virology, immunology, and mitochondrial biology, allowing him to develop a comprehensive understanding of the complex dynamics at play.
As Michita prepares to launch his own laboratory with support from the NIH Pathway to Independence Award, he is expanding his research to include HIV and its interactions with TNTs. His early experiments indicate that HIV-infected immune cells may also utilize these structures to invade placental cells, signaling a broader role for TNTs in maternal-fetal viral transmission.
The potential applications of his research are significant. By focusing on the NS1 protein, essential for TNT formation, Michita discovered that disabling NS1 in pregnant mice effectively protected their offspring from birth defects associated with Zika. This promising avenue of research could lead to new therapeutic strategies aimed at safeguarding maternal and fetal health.
As Michita reflects on his work, he remains enthusiastic about the future of virology and its implications for public health. “We could see NS1 traveling through TNTs. The movement was so clear, how they were traveling from one cell to another,” he remarked, emphasizing the clarity and excitement of observing these interactions in real time.
With his unique blend of curiosity, interdisciplinary knowledge, and commitment to addressing critical health issues, Rafael Michita is poised to make substantial contributions to the understanding of viral transmission and its impact on pregnancy. His work not only addresses immediate health concerns but also lays the groundwork for future research that could transform maternal-fetal medicine.
-

 Science1 month ago
Science1 month agoOhio State Study Uncovers Brain Connectivity and Function Links
-

 Politics1 month ago
Politics1 month agoHamas Chief Stresses Disarmament Tied to Occupation’s End
-

 Science1 month ago
Science1 month agoUniversity of Hawaiʻi Joins $25.6M AI Project for Disaster Monitoring
-

 Entertainment1 month ago
Entertainment1 month agoMegan Thee Stallion Exposes Alleged Online Attack by Bots
-
 Science4 weeks ago
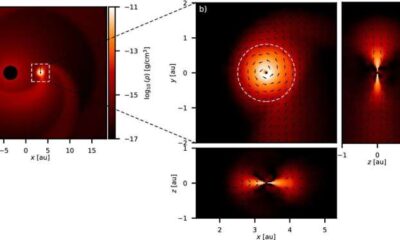
Science4 weeks agoALMA Discovers Companion Orbiting Giant Star π 1 Gruis
-

 Science2 months ago
Science2 months agoResearchers Challenge 200-Year-Old Physics Principle with Atomic Engines
-

 Entertainment1 month ago
Entertainment1 month agoPaloma Elsesser Shines at LA Event with Iconic Slicked-Back Bun
-

 World1 month ago
World1 month agoFDA Unveils Plan to Cut Drug Prices and Boost Biosimilars
-

 Business1 month ago
Business1 month agoMotley Fool Wealth Management Reduces Medtronic Holdings by 14.7%
-

 Top Stories1 month ago
Top Stories1 month agoFederal Agents Detain Driver in Addison; Protests Erupt Immediately
-

 Entertainment1 month ago
Entertainment1 month agoBeloved Artist and Community Leader Gloria Rosencrants Passes Away
-
 Science2 months ago
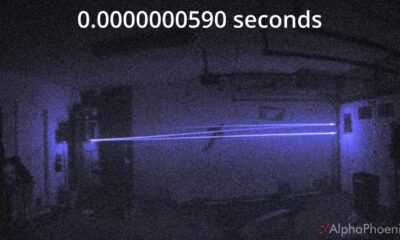
Science2 months agoInnovator Captures Light at 2 Billion Frames Per Second









