Top Stories
CDC Panel Limits Newborn Hepatitis B Vaccination; Urgent Concerns Rise

UPDATE: In a shocking move, the CDC’s Advisory Committee on Immunization Practices (ACIP) has voted to limit universal hepatitis B vaccination for newborns, triggering urgent concerns among health experts. The committee, in a 8–3 vote, will now only recommend vaccination for infants born to mothers who test positive for the virus. This decision was made without presenting new evidence to justify the significant change, raising alarms about the potential risks to newborns.
Health officials are highlighting the critical implications of this new policy. Currently, approximately 90% of infants infected with hepatitis B develop chronic conditions, leading to severe health issues including liver damage and an increased risk of liver cancer. José Romero, former ACIP chair, stated, “Delaying the birth dose would leave newborns unprotected during a critical window in their lives.” He emphasized, “Children will die preventable deaths without timely access to the hepatitis B vaccine.”
The controversial decision comes amid a tumultuous two-day meeting filled with heated debates and allegations that some ACIP members, appointed by Health and Human Services Secretary and antivaccine advocate Robert F. Kennedy Jr., sought to undermine the safety of the hepatitis B vaccine. These claims have been firmly refuted by a recent review from the University of Minnesota’s Vaccine Integrity Project, which analyzed over 400 studies and reinforced the vaccine’s safety and effectiveness.
Historically, universal hepatitis B vaccination was implemented in the United States in 1991, leading to a staggering 99% reduction in cases. The current recommendation shift could reverse decades of progress in protecting infants from this dangerous virus. Experts warn that without the immediate vaccination at birth, newborns face exposure not only from infected mothers but also from other caregivers, as the virus can remain viable on surfaces for over a week.
During the ACIP meeting, physician Jason Goldman, liaison for the American College of Physicians, cautioned that this change “will only endanger children.” In total, 18% of pregnant individuals do not receive hepatitis B screening, and many who test negative may still be at risk by the time of delivery. The delay in vaccination places infants in jeopardy during a critical period when they are most vulnerable.
Advocates for maintaining universal vaccination express grave concerns about the ethical implications of the new policy. Pediatric infectious disease specialist Cody Meissner, who voted against the change, stated, “We are doing harm.” He highlighted the moral imperative of the “do no harm” principle in medicine and warned against the consequences of this decision.
The public is urged to stay informed as health experts rally against what they view as a detrimental policy shift. The ACIP’s recommendations will be closely monitored, and further discussions are expected as the implications of this vote unfold. As the debate continues, the health and safety of millions of newborns hang in the balance.
As this story develops, readers are encouraged to share their thoughts and concerns about the potential impacts of these changes. The stakes are high, and the need for awareness is critical as we navigate this urgent public health issue.
-

 Science1 month ago
Science1 month agoOhio State Study Uncovers Brain Connectivity and Function Links
-

 Politics1 month ago
Politics1 month agoHamas Chief Stresses Disarmament Tied to Occupation’s End
-

 Science1 month ago
Science1 month agoUniversity of Hawaiʻi Joins $25.6M AI Project for Disaster Monitoring
-

 Entertainment1 month ago
Entertainment1 month agoMegan Thee Stallion Exposes Alleged Online Attack by Bots
-

 Science2 months ago
Science2 months agoResearchers Challenge 200-Year-Old Physics Principle with Atomic Engines
-
 Science3 weeks ago
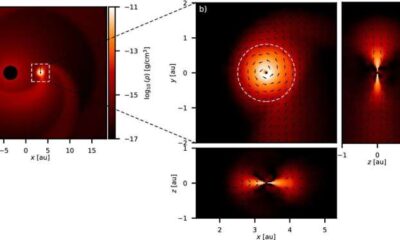
Science3 weeks agoALMA Discovers Companion Orbiting Giant Star π 1 Gruis
-

 Entertainment1 month ago
Entertainment1 month agoPaloma Elsesser Shines at LA Event with Iconic Slicked-Back Bun
-

 World1 month ago
World1 month agoFDA Unveils Plan to Cut Drug Prices and Boost Biosimilars
-

 Top Stories1 month ago
Top Stories1 month agoFederal Agents Detain Driver in Addison; Protests Erupt Immediately
-

 Business1 month ago
Business1 month agoMotley Fool Wealth Management Reduces Medtronic Holdings by 14.7%
-

 Entertainment1 month ago
Entertainment1 month agoBeloved Artist and Community Leader Gloria Rosencrants Passes Away
-

 Politics2 months ago
Politics2 months agoNHP Foundation Secures Land for 158 Affordable Apartments in Denver









