Health
Understanding Pollen-Food Allergy Syndrome and its Diagnosis

Pollen-Food Allergy Syndrome (PFAS) affects approximately 70% of individuals with pollen allergies, yet it remains largely unrecognized. This condition arises from cross-reactivity, where the body identifies proteins in pollen as similar to those in certain foods. When patients with pollen allergies consume foods containing these related proteins, known as Class 2 allergens, they may experience symptoms such as itching or swelling in the mouth, throat, and face, a reaction termed PFAS.
Diagnosing PFAS can be complex, but a detailed symptom history combined with specific IgE blood testing can clarify patients’ allergic triggers. This comprehensive approach enables healthcare providers to deliver tailored treatment plans, ultimately enhancing patients’ quality of life.
Overview of Pollen-Food Allergy Syndrome
PFAS is not uncommon, with estimates suggesting that more than 60% of food allergies stem from cross-reactions between food and inhaled allergens. Current data indicates that up to 20% of children and 58% of adults may be affected by this syndrome. The reactions vary depending on the type of pollen involved. For example, individuals allergic to birch pollen may experience symptoms after consuming foods like peaches, apples, and hazelnuts. Conversely, those with grass or weed pollen allergies may react to melons, bananas, and certain spices.
Geographical factors also influence the prevalence of PFAS. Specific pollen types are found in particular regions, which can trigger cross-reactivity. Understanding the link between pollen allergies and food reactions is crucial for effective diagnosis and management. Allergies to pollen lead to the production of antibodies against specific proteins. When these individuals consume certain plant foods containing similar proteins, their bodies react as if they encountered the pollen allergen.
The proteins responsible for PFAS are typically labile, meaning they are sensitive to heat and digestion. These proteins often undergo denaturation when heated or digested, which can reduce the likelihood of a reaction. Most PFAS symptoms are mild, but severe systemic reactions can occur in 2-10% of cases. These reactions may include nausea, abdominal discomfort, and anaphylaxis, making accurate diagnosis essential for effective management.
The Role of Patient History in Diagnosis
When patients report isolated symptoms in the oropharyngeal and upper gastrointestinal tract after consuming plant foods, it presents an opportunity for a thorough allergy assessment. A focused clinical history is the first step in this evaluation. If patients exhibit seasonal respiratory allergy symptoms, clinicians can create a comprehensive sensitization profile tailored to the individual’s geographic context. This profile assists in confirming pollen and environmental allergies, which informs a personalized management plan.
To assess suspected food allergies, clinicians should conduct specific IgE allergen sensitization testing, targeting the allergens indicated in the patient’s clinical history. If available, tests that include automatic reflexing to allergen components of the food are recommended. This method provides a detailed understanding of potential allergenic proteins to which patients may be sensitized, helping to identify primary allergies and cross-reactivities.
Correctly diagnosing PFAS, along with any concurrent pollen allergies, allows for informed management strategies. Patients can receive guidance on reducing environmental exposure to identified allergens, along with recommendations on how to prepare certain foods, such as peeling or cooking fruits and vegetables before consumption.
With up to 80% of allergy patients being allergic to more than one substance, understanding the cumulative impact of multiple allergens is crucial. Even if a patient has PFAS, they may also have one or more primary food allergies. A comprehensive assessment allows for a proactive approach to managing symptoms.
Prioritizing early and accurate allergy diagnosis is key to helping patients avoid unnecessary allergen exposure. With PFAS, a proper diagnostic approach transitions allergy management from a reactive to a proactive stance. This shift not only ensures better care but also significantly improves patients’ quality of life by minimizing allergen exposure and addressing symptoms effectively.
In conclusion, understanding and diagnosing Pollen-Food Allergy Syndrome is essential for improving health outcomes for those affected. By leveraging detailed patient histories and appropriate testing, clinicians can provide personalized strategies that enhance the lives of allergy sufferers.
-

 Science1 month ago
Science1 month agoOhio State Study Uncovers Brain Connectivity and Function Links
-

 Politics2 months ago
Politics2 months agoHamas Chief Stresses Disarmament Tied to Occupation’s End
-

 Science1 month ago
Science1 month agoUniversity of Hawaiʻi Joins $25.6M AI Project for Disaster Monitoring
-

 Entertainment1 month ago
Entertainment1 month agoMegan Thee Stallion Exposes Alleged Online Attack by Bots
-
 Science4 weeks ago
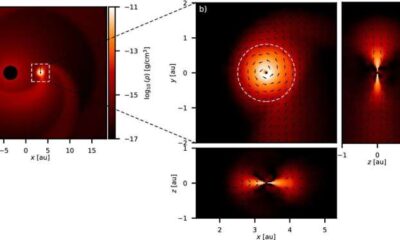
Science4 weeks agoALMA Discovers Companion Orbiting Giant Star π 1 Gruis
-

 Science2 months ago
Science2 months agoResearchers Challenge 200-Year-Old Physics Principle with Atomic Engines
-

 Entertainment1 month ago
Entertainment1 month agoPaloma Elsesser Shines at LA Event with Iconic Slicked-Back Bun
-

 World1 month ago
World1 month agoFDA Unveils Plan to Cut Drug Prices and Boost Biosimilars
-

 Business1 month ago
Business1 month agoMotley Fool Wealth Management Reduces Medtronic Holdings by 14.7%
-

 Top Stories2 months ago
Top Stories2 months agoFederal Agents Detain Driver in Addison; Protests Erupt Immediately
-

 Entertainment1 month ago
Entertainment1 month agoBeloved Artist and Community Leader Gloria Rosencrants Passes Away
-
 Science2 months ago
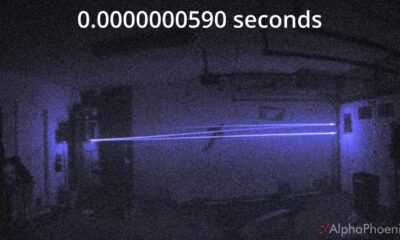
Science2 months agoInnovator Captures Light at 2 Billion Frames Per Second







