Health
MIT Develops Non-Surgical Brain Implants for Targeted Treatment

Researchers at the Massachusetts Institute of Technology (MIT) have made significant strides in developing non-surgical brain implants that could revolutionize the treatment of severe neurological conditions. The innovative technology involves microscopic, wireless bioelectronics that can travel through the bloodstream and autonomously implant themselves in specific regions of the brain. This advancement could drastically reduce the risks and costs associated with traditional surgical procedures for treating brain diseases.
In a study published on March 15, 2025, in the journal Nature Biotechnology, the team demonstrated how these tiny implants can identify and reach targeted areas in the brain without requiring human intervention. Once positioned, they can be wirelessly powered to deliver electrical stimulation, a process known as neuromodulation. This technique shows potential for treating conditions such as brain tumors, Alzheimer’s disease, and multiple sclerosis.
Deblina Sarkar, the AT&T Career Development Associate Professor in the MIT Media Lab and head of the Nano-Cybernetic Biotrek Lab, leads this research. She emphasizes that the circulatronics technology could make brain implants more accessible by eliminating the need for invasive surgery. The study’s lead author, Shubham Yadav, along with other collaborators from MIT, Wellesley College, and Harvard University, has contributed to this groundbreaking work.
Advancements in Circulatronics Technology
The research team has been exploring the concept of circulatronics for over six years. Each bioelectronic device is approximately one billionth the length of a grain of rice and made from organic semiconducting polymer layers sandwiched between metallic layers. These devices are fabricated at MIT’s advanced facilities and are integrated with living cells to form hybrids that can navigate the body.
The challenge of ensuring the electronics function properly after being detached from a silicon substrate took over a year to resolve. Sarkar noted, “The electronics worked perfectly when they were attached to the substrate, but when we originally lifted them off, they didn’t work anymore.”
The high efficiency of wireless power conversion is crucial for the devices’ operation deep within the brain. The researchers bonded the electronic devices with monocytes, a type of immune cell that targets inflammation. With the help of a fluorescent dye, they were able to trace the implants as they crossed the intact blood–brain barrier and self-implanted in the desired brain region.
Sarkar explains, “Our cell-electronics hybrid fuses the versatility of electronics with the biological transport and biochemical sensing prowess of living cells.” This unique integration allows the electronics to evade the body’s immune response and pass through the blood-brain barrier without invasive procedures.
Potential Applications and Future Directions
The tiny size of the circulatronics devices offers exceptional precision compared to conventional electrodes. They can self-implant, creating millions of microscopic stimulation sites that conform exactly to the shape of the target area. Importantly, the biocompatible devices can coexist with neurons without causing detrimental effects.
Through extensive biocompatibility testing, the researchers found that these implants can integrate safely with neural tissue without disrupting cognitive or motor functions. Once implanted, clinicians can use an external transmitter to deliver electromagnetic waves in the form of near-infrared light to power the devices and stimulate neurons.
The Sarkar lab is working to develop this technology for a variety of serious conditions, including brain cancer, Alzheimer’s disease, and chronic pain. The ability to treat glioblastoma, a challenging brain tumor that often presents in multiple locations, is particularly promising. Additionally, the technology may provide new treatment avenues for aggressive tumors such as diffuse intrinsic pontine glioma, which is typically inoperable.
“This is a platform technology and may be employed to treat multiple brain diseases and mental illnesses,” Sarkar states. The researchers aim to initiate clinical trials within three years through their startup, Cahira Technologies, and are exploring the integration of additional nanoelectronic circuits to enhance functionality.
Sarkar envisions a future where this technology not only addresses neural diseases that current therapies struggle to tackle but could also extend its applications beyond the brain to other parts of the body. She concludes, “Our tiny electronic devices seamlessly integrate with the neurons, creating a unique brain-computer symbiosis, and we are dedicated to employing this technology to alleviate human suffering.”
This research represents a significant leap forward in the quest for non-invasive solutions to some of the most challenging neurological conditions, potentially transforming patient care in the years to come.
-

 Politics1 week ago
Politics1 week agoHamas Chief Stresses Disarmament Tied to Occupation’s End
-

 Science3 weeks ago
Science3 weeks agoResearchers Challenge 200-Year-Old Physics Principle with Atomic Engines
-

 Science1 week ago
Science1 week agoOhio State Study Uncovers Brain Connectivity and Function Links
-

 Top Stories1 week ago
Top Stories1 week agoFederal Agents Detain Driver in Addison; Protests Erupt Immediately
-

 Entertainment1 week ago
Entertainment1 week agoMegan Thee Stallion Exposes Alleged Online Attack by Bots
-

 Entertainment2 weeks ago
Entertainment2 weeks agoSyracuse Stage Delivers Lively Adaptation of ‘The 39 Steps’
-

 World3 weeks ago
World3 weeks agoGlobal Military Spending: Air Forces Ranked by Budget and Capability
-

 Top Stories1 week ago
Top Stories1 week agoWill Smith Powers Dodgers to World Series Tie with Key Homer
-

 Politics3 weeks ago
Politics3 weeks agoNHP Foundation Secures Land for 158 Affordable Apartments in Denver
-

 Top Stories1 week ago
Top Stories1 week agoOrioles Hire Craig Albernaz as New Manager Amid Rebuild
-

 Lifestyle1 week ago
Lifestyle1 week agoTrump’s Push to Censor National Parks Faces Growing Backlash
-
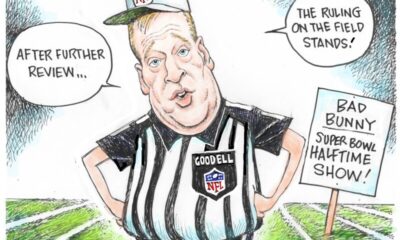
 Politics1 week ago
Politics1 week agoNFL Confirms Star-Studded Halftime Show for Super Bowl LVIII